- Table of Contents
- Overview
- Testimonials
- Withdrawal
- Addiction
- Resources
- Treatment
- Get Help Today
What are Benzodiazepines
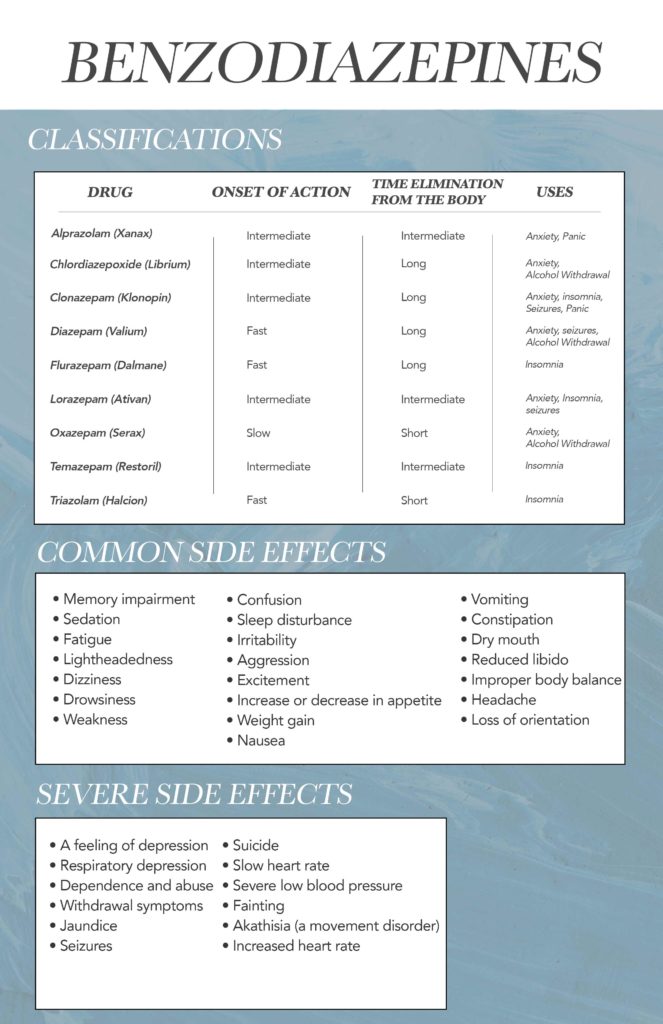
Benzodiazepines are a class of drugs typically used in the treatment of anxiety, but they can also be effective in treating several other conditions. Benzodiazepines, also known as “Benzos” man-made medications that cause mild to severe depression of the nerves within the brain (central nervous system) and sedation (drowsiness). They work by affecting neurotransmitters in the brain, more specifically the GABA (gamma-aminobutyric acid) neurotransmitter. Scientists believe that the cause of anxiety and other psychological disorders may be the result of excessive activity of the nerves. When these medications enhance the effects of GABA neurotransmitters, the CNS is depressed and therefore reduces the activity of the nerves in the brain resulting in a more relaxed state.
Benzodiazepine Interactions with Other Drugs
Benzodiazepines are depressants, so when combined with other depressants – alcohol, barbiturates, narcotics, and tranquilizers – this can lead to excessive sedation. This excessive sedation typically causes depressed breathing, slowed heart rate, and mental impairment. In some cases, these effects can so severe to the point they become life-threatening.
Some benzodiazepines like alprazolam (Xanax) and diazepam (Valium) when combined with certain drugs like valproic acid (Depakene, Stavzor), ketoconazole (Nizoral, Xolegel), cimetidine (Tagamet) can slow the elimination of drugs in the liver. Reduced elimination may result in unintended effects of increased blood concentrations.
Drinking with benzodiazepines is extremely dangerous! It’s not safe to drink alcohol or take other drugs that have similar effects on the central nervous system (CNS) at the same time because these drugs or substances interact with oral benzodiazepines by causing additional depression of the brain and respiratory depression. Respiratory depression can lead to breathing that’s inadequate for supplying oxygen to the body which is a very common cause of overdose deaths.
Withdrawing from Benzodiazepines
Benzodiazepines are not intended to be taken regularly for a long period of time. If a person uses this drug for a prolonged period of time they will develop both a physical and psychological dependence to the drug. The amount of time the body forms a dependence depends on a variety of factors: psychological dependence can form the first time a person uses the drug; physical dependence depends on how long and often the person is using the drug.
When a person stops taking the benzodiazepine after using it for an extended period of time a person may feel feelings of loss of self-worth, agitation, and insomnia. If benzodiazepines are taken continuously for longer than a few months, stopping therapy suddenly may produce seizures, tremors, muscle cramping, vomiting, and sweating. In order to avoid withdrawal symptoms, the dose of benzodiazepines should be tapered slowly.
Withdrawal symptoms
The symptoms of withdrawal vary between the specific benzodiazepine taken. A general rule of thumb is the withdrawals will often increase what the drug suppresses to the body. For instance, valium is prescribed for anxiety, muscle relaxation, and seizures; so once a person stops taking valium, the risks for these symptoms are increased. General symptoms of benzodiazepine withdrawal include:
- Palpitations
- Dry heaving and vomiting
- Sleep problems
- Muscle pain and stiffness
- Increased anxiety and tension
- Headache
- Panic attacks
- Hand tremors
- Irritability
- Problems concentrating
The severity of the withdrawal symptoms depends on the amount and duration of benzodiazepine use but withdrawal symptoms can sometimes be deadly. Severe withdrawal symptoms of Benzodiazepines include:
- Seizures
- Psychosis or psychotic reactions
- Increased risk of suicidal ideation
- Severe Depression
Withdrawal Timeline
There is not a specific timeline for benzos as it depends on a variety of factors like:
- Length of time taking benzodiazepines
- Dosage amount
- Type of drug used/abused
- The method used to take or abuse benzodiazepines
- Underlying medical or mental health issues
- Abuse of other drugs or alcohol concurrently
For example, Valium has a long half-life - meaning it takes longer for the drug to leave the body - therefore the symptoms of withdrawal will last longer but may not present themselves until later. On the other hand, benzos like Xanax – which have a shorter half-life but are typically more potent than some long acting ones – will have more intense withdrawals at a quicker rate.
Early withdrawal
usually starts within a few hours to a few days of stopping the medication and may last a few days. During early withdrawal, an individual may experience a return of anxiety and insomnia symptoms as the brain rebounds without the drugs. Symptoms the benzos worked to suppress may come flooding back. The tapering process frequently used in medical detox may help dampen this rebound effect.
Acute withdrawal
After a few days of stopping a benzodiazepine, acute withdrawal may begin. This phase constitutes the bulk of withdrawal. Symptoms may include anxiety, panic, insomnia, muscle spasms or tension, nausea and/or vomiting, diarrhea, blurred vision, seizures, hallucinations, short-term memory impairment, trouble concentrating, clouded thinking, mood swings, agitation, drug cravings, twitching and weight loss due to a decreased appetite. It is during this phase that specific medications may be most beneficial at targeting some of the certain symptoms. Suicidal thoughts and actions may occur during acute withdrawal from a benzodiazepine as well, and therapy and support groups may help diffuse these complicated emotions. Acute withdrawal may last between two weeks and several months.
Protracted withdrawal.
Some people, around 10 percent according to a study published by ABC News, may experience protracted withdrawal syndrome that can extend several months or even years after stopping the use of a benzodiazepine.
Individuals may experience tingling in their arms and legs, muscle twitches, prolonged anxiety and insomnia, and cognitive deficits as well as depression and mood swings that may be difficult to manage. These symptoms may appear randomly and without warning. Mental health services and support beyond medical detox include therapy and counseling to manage protracted withdrawal symptoms. When a mental health disorder is also present, called co-occurring disorders, specialized treatment that caters to dual diagnoses may be beneficial during recovery.
Treatment for Benzo Withdrawal
By gradually tapering their dose, a person can usually avoid severe withdrawal. But withdrawing from benzodiazepines on your own can be difficult and is best handled with the help of medical professionals.
A medically managed detox can provide you with the support and medical care to safely stop using benzodiazepines. Benzo detox can be handled on either an inpatient or outpatient basis depending upon the severity of your dependence.
Your physician will likely devise a detox schedule to gradually reduce your doses over several weeks or several months.
Alternatively, your doctor may decide to switch you to a longer-acting benzodiazepine, such as diazepam, and then gradually wean you off that. This will minimize symptoms and prevent withdrawal complications while your body and brain readjust.
Both of these methods of benzodiazepine withdrawal treatment are endorsed in the Ashton Manual, a guide written by Dr. Heather Ashton, former emeritus professor of clinical psychopharmacology at the University of Newcastle upon Tyne, England.
The Ashton method takes into account the various factors — including the type of benzo, the duration of use, and the dose taken — that affect patterns of withdrawal among benzo-dependent people and offers several withdrawal schedules that can be adapted as needed.
Individuals with severe withdrawal symptoms or a high risk of complications may require hospitalization. With inpatient treatment, you’ll receive round-the-clock monitoring and therapeutic support. You’ll also receive medications to help combat nausea, insomnia, anxiety and withdrawal-related symptoms.
After completing detox, you’ll be ready to begin the next steps of benzo treatment.
Quitting benzodiazepines can be grueling, but a successful detox is your best hope for beating benzodiazepine dependence. According to a 2018 review in the Journal of Clinical Medicine, recovery success rates can approach 70 to 80 percent when benzodiazepine withdrawal is properly managed.
Benzodiazepine Addiction
These medications are classified by the Drug Enforcement Administration (DEA) as Schedule IV drugs. This schedule of drug often poses high risks for dependence. Therefore, people who take benzos regularly (prescribed or illicitly) will eventually develop a physical and psychological dependence to the drug. Those who stop taking the drug after dependence has developed will experience harsh withdrawal symptoms; some even fatal. Always talk to a medical professional before quitting benzo use. While most people will develop dependence after continued use, only some individuals develop an addiction.
Addiction is another term for a severe substance use disorder. It’s a disease of the brain that causes repeated drug use despite negative consequences. When benzodiazepines are used correctly and as prescribed they are safe and effective but those who abuse benzos are often susceptible to addiction.
Signs of Benzo Addiction
- The person withdraws from friends, family, and obligations in order to use the drug.
- From a place of fear of being without the drug, the person ensures that an adequate supply is maintained at home.
- The person does uncharacteristic things to be able to pay for the drug, such as borrowing money, stealing, draining bank accounts, or maxing out credit cards.
- The person engages in risky activities, such as driving, after using the drug.
- The person exhibits a reduction in effort to maintain hygiene or grooming (i.e., the person may begin to look disheveled).
- The person is uncharacteristically secretive about daily schedule and/or tells lies to protect the substance abuse.
- Shifts in mood or personality are experienced.
Consequences of Benzo Addiction
Drug Overdose (Death)
The most severe form of physical harm caused by a benzodiazepine occurs during an overdose. This occurs when a person takes too much of the drug at once and overloads the brain and body. This can be especially common after the body forms a dependence and requires more and more to feel the same desired effects. The Centers for Disease Control and Prevention (CDC) cites drug overdose as the number one cause of injury death in the United States.
Memory Impairment
Benzodiazepines may interfere with cognition and memory when used regularly for an extended amount of time. Benzodiazepines are thought to particularly interfere with visuospatial abilities, processing speed, and verbal learning abilities, as published by the Journal of Clinical Psychiatry.
Fortunately, many of the changes made by benzodiazepines to the different regions of the brain after prolonged use may be reversed after being free from these drugs for an extended period of time.
Relationship Damage
Personality changes often accompany drug abuse and addiction. For example, some people experience a lack of impulse control that they did not previously exhibit.
Legal Entanglements
Law problems may result from benzodiazepine abuse, especially when it comes to certain formulations of these drugs. Flunitrazepam is the only benzodiazepine that is treated as a Schedule I drug in the court system. This means that the legal consequences for illicitly using, possessing or distributing this particular benzodiazepine are far more severe than those associated with all other benzodiazepines in Schedule IV.
Career or Academic Damage
In addition to the all-consuming drug-seeking behaviors that accompany addiction and detract from other important areas of life, long-term benzodiazepine abuse has been shown to cause brain damage and reduced mental function. Job loss may result. Students may fail to reach their academic goals, such as earning a college degree.
Addiction Resources
Benzodiazepine Addiction Treatment
For the most part, treatment from benzo use disorder is relatively standard. It begins with a detox procedure and leads into a combination of medication, education, therapy and counseling; and life coaching. Through these mediums, a treatment center helps heal the various aspects of addiction by focusing on the underlying symptoms that cause a person to abuse the drug.
Not everyone’s treatment path is going to be the same. For instance, some people may have anxiety and PTSD alongside their addiction. Having both anxiety and a substance use disorder is considered a “co-occurring disorder.” To effectively treat each and both effectively, a treatment center should be considered “dual-diagnosis” meaning they can treat each disorder separately but at the same time. This is extremely important as many medications used to treat mental illnesses can be susceptible to dependence and abuse. Therefore, knowing a person has a substance use disorder while prescribing medications for their anxiety can help limit their potential for abuse in the future.
When a person abuses their prescribed medication like Xanax for addiction; it poses a problem. To fully treat the underlying symptoms of abuse, the mental health concerns – in this case, Anxiety – need to be addressed alongside the substance use disorder to treat the individual effectively. This can cause a problem as the medications typically prescribed are the exact drugs he or she is abusing. Here are some ways Dual-Diagnosis treatment centers solve this dilemma.
Benzodiazepines Alternatives: Antidepressants
In general, antidepressants, especially selective serotonin reuptake inhibitors (SSRIs) such as sertraline (Zoloft), are as effective as and safer than benzodiazepines for the long-term treatment of panic disorder and generalized anxiety. Antidepressants have the advantage of relieving depression as well as anxiety, and they create less risk of dependence. But because antidepressants take weeks to work, benzodiazepines are often prescribed to tide patients over. The dose of the benzodiazepine is gradually reduced as the antidepressant takes effect.
Benzodiazepines Alternatives: Other drugs
Buspirone (BuSpar), used in the treatment of chronic anxiety, enhances the effect of the neurotransmitter serotonin. It is less effective than benzodiazepines and takes longer to work (several weeks), but it is less likely to cause physical dependence.
Ramelteon, a recently introduced treatment for insomnia, acts at receptors for melatonin, a hormone that helps to regulate the body’s circadian (24-hour) cycles. It is approved for long-term use.
Antihistamines are over-the-counter drugs sometimes used as sedatives. Diphenhydramine (Benadryl) is the most widely available. Side effects include daytime drowsiness and blurred vision.
Benzodiazepines Alternatives: Treatment without drugs
Exercise, muscle relaxation training, yoga, breath training, and hypnosis can be used to relieve both insomnia and anxiety. Psychotherapy of various kinds is helpful for the long-term treatment of both. The most carefully studied and often the best alternative to benzodiazepines and related drugs is cognitive-behavioral therapy.
For insomnia, the cognitive-behavioral approach involves recording and changing both sleep habits and ways of thinking about sleep. Patients learn to go to bed only when sleepy, to exercise regularly but not near bedtime, to avoid eating, reading, or watching television in bed, and to rise at the same time no matter how little they have slept. They learn how to use relaxation techniques and breathing exercises, visualize soothing scenes or repeat neutral sounds to fall asleep. They also learn to recognize and change unrealistic ideas, such as the belief that they will never be able to sleep well without drugs.
In the cognitive-behavioral treatment of anxiety, patients record, examine, and analyze their thoughts and feelings, with special attention to those that provoke or relieve anxiety. While the therapist helps them to become aware of unrealistic thinking, they also learn new ways to respond to anxiety-provoking situations and practice the techniques of exposure and systematic desensitization.
In most studies, cognitive behavioral therapy is found to be as effective as benzodiazepines and other medications, and its impact often lasts longer. A combination of drugs and cognitive behavioral therapy may be more effective than either alone. But in some studies of insomnia, cognitive behavioral therapy alone has been found superior to the combination, possibly because patients are less committed to the behavioral and cognitive techniques if they know they can fall back on a drug.
Cognitive-behavioral therapy has few risks. Its main disadvantage is that it requires training and experience that many clinicians lack.
Medically Reviewed By:

Coalition Recovery’s 4x Board Certified Psychiatrist in Addiction, General, Forensic & Geriatric Psychiatry.






